The costs of vaccine hesitancy
As U.S. insurance providers and hospital networks reckon with the “preventable costs” of vaccine hesitancy, should employers consider doing the same?
According to the Centers for Disease Control and Prevention, 86.3% of the U.S. adult have received at least one dose of the COVID-19 vaccination. Of those unvaccinated, 10.1% say they “probably” or “definitely will not” get vaccinated.
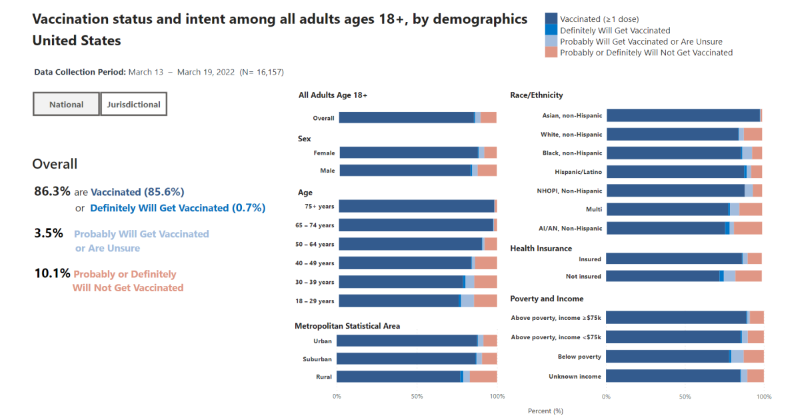
Time reports that fewer than 80,000 adults are receiving a first vaccination dose each day at this point, and most of those are occurring within marginalized communities: Black and Hispanic people, people without insurance, LGBTQ people and those living in under-resourced counties. Community health organizations say the initial federal vaccine rollout did not go far enough on offering personal outreach, information and support to those communities, though grassroots health organizations are continuing that work.
While 3.5% of U.S. adults may still get vaccinated, a picture of the economic cost of vaccine hesitancy is beginning to emerge according to Reuters. And that picture isn’t pretty.
A December study by the Kaiser Family Foundation, which tracks U.S. health policy and outcomes, estimated that unvaccinated Americans accounted for $13.8 billion in “preventable” COVID hospitalization costs nationwide between June and November 2021. There are also concerns about the financial drain on programs such as Medicare.
For employers, vaccine hesitancy can contribute to short-staffed workplaces. Some employers may also be considering a risk premium to unvaccinated workers, similar to how people who smoke may be required to pay higher health premiums.
Vaccines make COVID hospitalizations “preventable”
Vaccines have proven to be effective against the virus, with CDC figures from the Delta wave in 2021 revealing that unvaccinated Americans had four times greater risk of being infected and nearly 13 times the risk of death. The Kaiser Family Foundation study also estimates that between June and November 2021, which included the Delta wave, vaccinations could have averted 59% of COVID hospitalizations among U.S. adults with an average cost of $20,000 each.
As U.S. insurance providers and hospital networks experience the ramifications of vaccine hesitancy, it’s likely more health-related costs will be passed down. As it is, Reuters says most private health insurers have stopped waiving deductibles or cost-sharing for hospitalizations caused by COVID-19 — a change from earlier in the pandemic.
Because of the availability of COVID-19 vaccines and their effectiveness, insurance companies are passing along more of the costs to patients. Some countries, such as Greece and Singapore, are also taking a stance by implementing fines, fees and not covering medical bills for the unvaccinated. Should employers do the same?
Up to employers
The only nationwide vaccine mandate in effect is the Centers for Medicare and Medicaid Services vaccination mandate for certain employees at hospitals, nursing homes and other health care providers that receive federal funds, which was upheld by the U.S. Supreme Court earlier this year.
New York City’s private-sector vaccination order remains in effect, though Mayor Eric Adams has indicated he expects to eventually roll it back (and has rolled it back for nonresident professional athletes and performers). Some states, like Indiana, are going the opposite direction and adopting rules that prevent or restrict workplace COVID-19 vaccination mandates.
All this puts the onus on employers to determine a path forward. Some employers have begun announcing cost impacts for the unvaccinated, including:
- J.P. Morgan and Bank of America informed U.S. employees to expect to pay more or receive fewer perks through company wellness programs unless proof of vaccination can be shown.
- Delta Airlines announced an extra $200 a month charge for health insurance for unvaccinated employees.
- Utah grocer Harmons also has an insurance premium surcharge up to $200 per month that applies to “unvaccinated associates who don’t qualify for an exemption or who chose not to complete a vaccine education series.”
If considering implementing your own insurance discount or surcharge for COVID-19 vaccinations, law firm Jackson Lewis outlines a few issues to consider:
- How much will the surcharge or discount be?
- How does a vaccination surcharge or discount interact with other wellness incentives offered?
- Will the surcharge only apply for vaccine hesitant employees or also for any spouses or dependents also on the health plan?
- What reasonable accommodations need to be made under either the Americans with Disabilities Act or if vaccination is medically inadvisable for an employee?
- Should boosters be required?
While much remains unknown about the future of the COVID-19 pandemic as variants continue to emerge, vaccine hesitancy has had a cost. The question now is who should and will continue to pay it?
COMMENT
Ragan.com Daily Headlines
Tags: COVID-19, health care, healthcare costs, unvaccinated workers, vaccination






